news
Setting Yourself Apart: Why Professional Certifications Matter
You have been working as a provider recruitment professional for a few years. While you know what the job entails; just how deeply do you understand your role? How well do you know the roles others play in your success? How confidently do you represent physician and provider recruitment when working with the C-suite?
Reviewing these questions, could you confidently say you are strong in all these areas? If so, maybe you have completed the Certified Physician Recruitment Professional course through the Association for Advancing Physician and Provider Recruitment.
There is good news, however, if you cannot positively say you are proficient in all these areas. AAPPR is able to help you to develop into a stronger and more confident physician and provider recruitment professional through our CPRP certification program. The CPRP certification program encourages professionals to develop the skills they already have in the field of physician and provider recruitment and to provides them with additional knowledge.
Certification Versus Certificate
Before understanding why professional certification matters, we must understand what it is and how it differs from a certificate.
The key difference between a certification and a certificate lies in the level of recognition and the requirements involved. Certifications typically represent a higher level of expertise and requires meeting specific standards, often set by professional associations such as AAPPR. Typically, certifications require continuing education to maintain the certification and require those who hold the certification to periodically renew it. On the other hand, certificates signify the successful completion of a training program, course, or workshop without necessarily meeting the stringent criteria associated with certifications such as an examination or continuing education. Both can be valuable in different contexts, depending on the individual’s goals and the industry’s requirements.
What is CPRP?
At its core, the Certified Physician Recruitment Professional program has an instructional design based on the AAPPR Competency Model’s technical and cross-cutting domains. Each competency has learning objectives based on physician and provider recruiters’ roles. The course breaks down the tasks recruitment professionals must be proficient in and provides the knowledge needed to fully understand the learning objectives.
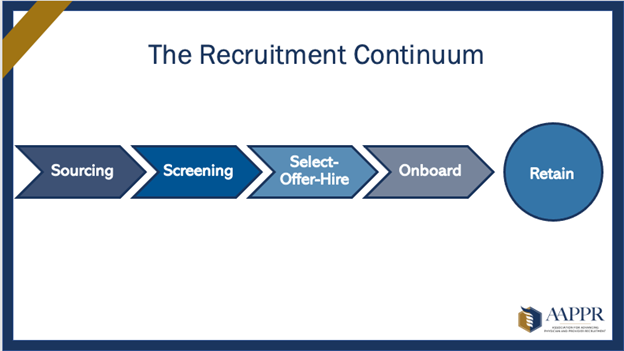
The course provides an in-depth view of recruiting basics such as sourcing, screening, and interviewing, as well as delving deeper into advanced topics such as interpreting benchmarking metrics and understanding/implementing medical staff development plans. Recruitment professionals who pass the exam at the end of the course to earn the CPRP certification are equipped with resources, best practices, and cutting-edge training that are used every day to recruit and retain top candidates for their hospital and health systems and influence hiring practices in the provider workforce.
What is the AAPPR Competency Model?
AAPPR is committed to continually advancing the recruitment profession and addressing the entire continuum of physician and provider recruitment. To acknowledge changes the recruitment profession has undergone, and to focus its professional development efforts in the future, AAPPR developed a competency model. This model then used to develop the CPRP program.
The competency model defines the skills and knowledge required for recruitment professionals to be successful now and in the future. It serves as the foundation of AAPPR’s core curriculum and illustrates what recruitment professionals need to know now and in the future.
The Competencies
Source
Source: identifying and/or building a provider prospect pool and creating awareness of/interest in practice opportunities.
Among the tasks in Source are researching specialty trends and market data and recommending and implementing a broad-based diverse sourcing strategy to identify a pool of qualified candidates. The learning objectives include identifying requirements for physician and advanced practice provider education, credentialing, and licensing and knowing the sources of specialty trends and market data applicable to sourcing strategy.
Screen
Screen: the internal process of pre-qualifying candidates to meet organizational/provider expectations, which may include interviews and site visits.
The tasks for practicing recruitment and retention defined under this objective include adherence to legal and regulatory requirements and organizational policies, the recommendation of whether or not to proceed with the prospect as a candidate, and coordination of the candidate’s site visit itinerary. The learning objectives include identifying critical elements involved in and appropriate approaches to evaluating the applicant’s application for fit to the position and identifying the essential elements involved in and proper procedures to verify licenses and credentials. You must also assess whether screening approaches comply with key laws and regulations.
Select, Offer, and Hire
Select, Offer, and Hire: the process between identifying and selecting the best fit candidate through the extension and closing of an offer.
Tasks under this objective include gathering evaluations from interviewers and the candidate and summarizing and sharing the evaluation feedback with decision-makers. Learning objectives include identifying the critical elements involved in and appropriate approaches to the verbal officer, letter of intent, contract, and service agreement.
Onboard
Onboard: continuing the recruitment process to meet onboarding timelines and standards, ensuring successful entry and integration into practice and community.
The tasks are to coordinate the handoff of the selected candidate with responsible onboarding contacts and to ensure the timely completion of onboarding tasks with the selected candidate.
Learning objectives include applying IRS regulations regarding physician and provider relocation and evaluating whether onboarding approaches comply with critical laws and regulations while also meeting the needs of the candidate to successfully integrate into the organization.
Retain
Retain: data analysis, strategic alignment, and program implementation with the intent of promoting provider satisfaction, resulting in increased retention.
Tasks under Retain are to support and implement organizational provider retention strategies as defined by recruitment and retention leadership. Learning objectives include identifying sources of specialty trends and market data beneficial to retention strategy.
Plan for Workforce Succession
Plan for Workforce Succession: data analysis, strategic alignment, and program implementation to create a viable pipeline for workforce succession.
These tasks are to alert recruitment and retention leadership to potential staffing needs and market influences. Learning objectives are to identify sources for trends in the labor market and workforce planning and to identify critical elements of a medical staff development plan.
Practice Professionally and Ethically
Practice Professionally and Ethically: driving a professional and ethical environment.
Tasks under this section include working within personal and professional limitations and abilities and identifying and taking appropriate steps to maintain and enhance competence.
Learning objectives include recognizing the importance of maintaining and enhancing competence, identifying sources of learning for recruiters, and evaluating whether a situation presents a conflict of interest.
Communicate to Establish and Maintain Relationships
Communicate to Establish and Maintain Relationships: fostering and building trust internally and externally.
Tasks include providing proactive communications to report accurate information and reliable data. Learning objectives are recognizing effective communication techniques to avoid confrontations and resolve conflicts. A second objective is the ability to understand effective coaching and influencing techniques.
Champion Equity, Diversity, and Inclusion
Champion Equity, Diversity, and Inclusion: activities that create synergy and incorporate diverse provider demographics to create value for internal and external stakeholders.
Tasks include developing diverse and inclusive sourcing and screening strategies and coaching internal hiring authorities and recruitment participants on inclusion and diversity policies and best practices. Learning objectives include recognizing barriers to equity, diversity, and inclusion. They also include identifying and recognizing implicit and unconscious bias types and how they can influence recruitment and retention efforts.
Use Data in Decision-Making
Use Data in Decision Making: research, retrieval, analysis, and reporting relevant facts and figures leading to evidence-based solutions.
The task requires the use of data in decision-making, including using it to remove bias in the screening/interview process (such as objective vs. subjective candidate matrix). Recruiters also will use labor market data to assess external forces on provider recruitment and retention (supply/demand, third-party salary data, and external turnover). Learning objectives include the ability to identify the critical elements involved in and appropriate approaches to converting data points into meaningful measures. Also, recruiters must identify the key factors involved and proper methods for comparing collected data to national benchmarks.
Setting Yourself Apart
Physician and provider recruitment professionals usually find themselves in the profession because they have specific natural skills that make them a good fit for the job. While some may have a Business Management, Healthcare Administration, or Human Resources degree, there isn’t a formal degree program for physician and provider recruitment. However, this doesn’t mean that individuals aren’t required to have the necessary skill sets to succeed.
As the leader in physician and provider recruitment, AAPPR offers recruitment professionals the opportunity to demonstrate the value of their skills and continually hone their abilities through the CPRP certification program.
The CPRP certification proves that a recruitment professional has acquired the knowledge and skills required to perform their roles to the highest standard. It demonstrates expertise in the field of provider recruitment but also a commitment to the profession.
By obtaining your professional certification, you signal that you are committed to the profession and are dedicated to maintaining a high level of competence. Because the field of physician and provider recruitment is continually the CPRP certificate requires holders to renew their certification every three years through continuing education. By committing to ongoing professional development, those with the certification stay current with the latest industry trends and technologies and demonstrate their commitment to further advancing the profession.
Professional certifications such as CPRP will help you to stand out in the field and industry. It shows that you are committed to the profession and demonstrates your expertise – setting you apart and placing you at the top of the industry.