Have a question?
Contact us
The Association for Advancing Physician and Provider Recruitment (AAPPR) is redefining recruitment to retention and is the only professional organization where physician and provider recruitment leaders and others who influence recruitment, onboarding and retention can connect, learn and advance their careers.
With the ongoing national physician shortage, physician and provider recruitment professionals are well aware of how it will continue to impact the workforce. The American Association of Medical Colleges projects a national shortfall of anywhere between 37,000 to more than 100,000 physicians over the next decade, meaning effective recruitment strategies are extremely vital to healthcare systems’ ability to provide quality care to future patients. As the search for talent becomes increasingly competitive and challenging, first impressions are critical, and this often comes in the form of a job posting.
What do physicians want?
At AAPPR’s annual conference, Advancing Connections, Jacob Simon of The Medicus Firm shared valuable insights on physician preferences and the type of information that affects their career decisions.
According to the firm, the top three motivating factors for both physicians and APPs to make a career change are work/life balance, compensation and location. Another common factor that motivates physicians – especially those early in their career – is the opportunity to grow within an organization. Recruitment professionals should consider these motivating factors within recruitment and retention strategies.
Five things to include in a job posting
It’s important to prioritize physicians’ motivating factors when considering the details to include in a job posting. To catch candidates’ eye and gain their interest in an opportunity, job postings should be transparent and include the following:
There is an immense amount of competition for talent in the healthcare community. Recruitment professionals need to put their best foot forward in job postings in order to grab candidates’ attention and support them in taking the next step in their career.
By aligning job posting details with physicians’ interests, recruitment professionals can not only attract high-quality candidates, but ensure that candidates are well-informed in their decision to apply to organizations that align with their own unique needs and values.
Recruitment is a fast-paced industry. Especially healthcare recruitment where there is a shortage in supply of candidates while the demand is extremely high. Healthcare recruiters often have no choice but to answer that physician candidate after 6pm or on a Saturday when the candidate is finally free from patient care. Never mind recruiters have a family of their own and well deserved precious personal time to enjoy.
This is why it is so important for all of us to work on Self-Care.
Remember, self-care is not selfish; it’s essential for your long-term well-being and success as a recruiter. By prioritizing your physical and mental health, you’ll be better equipped to handle the demands of your job and achieve greater job satisfaction.
Survey shows high satisfaction with work-life balance, while average salary reaches four-year low
The Association for Advancing Physician and Provider Recruitment (AAPPR) has released its 2024 Recruitment Team Professional Compensation Benchmarking Report, highlighting detailed profile and compensation information on internal physician and provider recruitment professionals.
Among key findings in the report, nearly three quarters of recruitment professionals are somewhat or completely satisfied with their current position and role, and 70 percent reported “Good” or “Excellent” work/life balance. However, respondents’ satisfaction with their compensation decreased from 67 percent in 2019 to 55 percent in 2023.
“The benchmarking data shows that while flexibility and work/life balance are improving in the recruitment profession, workplace stress is still high across the board and compensation remains unsatisfactory for many in our field,” said Carey Goryl, CEO of AAPPR. “The average salary in this year’s report is the lowest since 2019 and down 4 percent since last year. Amid the national physician shortage, we need to ensure that organizations recognize recruitment professionals’ important and challenging work, and their contributions to organizations’ ability to deliver quality care in their communities.”
The report includes two chapters highlighting survey results related to physician recruitment profiles and compensation levels. The first chapter, “Internal Physician and Provider Recruiter Profile Statistics,” provides data on demographic information, including recruitment professionals’ roles, education levels and responsibilities. A total of 545 physician recruitment professionals from 104 organizations participated in this survey.
The second chapter, “Internal Physician and Provider Recruiter Compensation,” examines compensation levels of recruitment professionals by their role, experience, education level, etc. This survey had participation from 95 organizations and collected data from 476 recruiters.
Some notable findings include:
The industry-level data in AAPPR’s benchmarking surveys helps recruitment professionals and departments establish target productivity levels, set goals and expectations and grow their teams.
Organizations that participated in the annual survey received a complimentary copy of the report and free access to AAPPR’s Benchmarking Portal, enabling them to run custom benchmark comparisons against similar organizations and departments. The Benchmarking Portal includes time to fill and compensation calculators and enables users to compare a range of data, including organizational profiles, search information, recruiter profile data, and recruiter compensation figures, helping them make more informed decisions.
The complete AAPPR 2024 Recruitment Team Professional Compensation Benchmarking Report is available for purchase at https://aappr.org/research/benchmarking/.
About The Association for Advancing Physician and Provider Recruitment (AAPPR)
The Association for Advancing Physician and Provider Recruitment (AAPPR) is a nationally recognized leader in health care provider recruitment, onboarding, and retention. For more than 30 years, AAPPR has empowered physician and advanced practice provider recruitment leaders to transform care delivery in their communities by providing best-in-class practices, up-to-date industry knowledge, and evolving innovative approaches for hiring, onboarding, and retaining exceptional clinical talent. To learn more or to become an organizational member of AAPPR, please visit https://aappr.org/join-now.
Along with the evolution of healthcare, the needs of the physician and provider workforce are quickly changing due to generational differences, a need to address high burnout rates and the ongoing physician shortage.
In fact, AAPPR research shows that 28% of physicians who resigned from large healthcare organizations (those with 1,000 or more providers) in 2021 cited burnout as a primary driver for their decision.
The future physician workforce places a premium on flexible hours, work-life balance, and integrated technologies that enhance their day-to-day efficiency and quality of care. With these evolving needs in mind, healthcare systems must adapt to and accommodate physicians’ priorities to remain competitive and bring high quality and effective care to patients.
AAPPR CEO Carey Goryl recently moderated a panel of board members Allan Cacanindin and Marjorie Alexander, and JT Thoms, National Account Executive at Jackson and Coker LocumTenens, to discuss the critical connection between technology and the evolution of the physician landscape at the HIMSS 2024 Annual Conference. The industry experts shared their advice for how recruitment professionals can stay ahead of the curve as the industry faces increasing hurdles. Here are our key takeaways:
Burnout among current staff can be detrimental to a workforce that’s already experiencing a significant shortage. That’s why improving flexibility and providing candidates and current employees with the work-life balance they are consistently craving is so important. To do this, organizations should adopt technology that actively monitors the times physicians are entering their notes into EHR platforms and flagging providers who routinely enter notes after hours. This practice gives leaders a better understanding of team members consistently working outside of their normal hours, so they can then lend support if needed to ensure all providers are able to finish their workday by 5 p.m. Small changes like this can be instrumental in ensuring physicians have greater work-life balance and helping to reduce burnout.
While not necessarily technologically innovative, we can’t overstate the importance of talking to the people who are choosing to stay at your organization. To understand physician needs, current burnout levels and ultimately reduce turnover, leaders should regularly conduct stay interviews with their employees. These interviews can be held by leaders who do not directly manage the provider, with the objectives of monitoring wellbeing, identifying positive and negative feedback from providers and creating an open dialogue to ensure needs and concerns are discussed before they result in a resignation. Most importantly, leaders and recruitment professionals should be sure to track the data that is collected during these stay interviews and implement findings in a way that continues to support the needs of your organization’s workforce.
A common cause of burnout among physicians and providers is the level of manual administrative work required every day. Technology, from AI and telehealth to smartphone applications that make physicians’ work easier, have the potential to reduce burnout, increase physician efficiency and align with the preferences of younger physicians who are accustomed to using technology in their everyday lives. Not only can technology help physicians streamline their everyday practices and spend time where it matters the most, but an increasing use of technology will also become critical across recruitment operations. Implementing the right technologies at your organization can support faster processes, identify rates of provider productivity and create efficient pathways for solution planning to evolve your clinical workforce strategies.
The United States could see a physician shortage of between 37,800 – 124,000 physicians by 2034, according to data published by the AAMC (Association of American Medical Colleges). This drastic shortage, plus the evolving landscape of existing physicians’ expectations and needs, are challenging physician and provider recruiters to innovate like never before. With a decreasing number of physicians serving an increasing need for healthcare, recruitment professionals must look to adopt new ways to meet clinicians’ evolving needs so they can continue to best serve patients.
Every person has a different approach to listening, learning, and working. Having different thought processes, different backgrounds, and different ways of communicating is essential in the workplace. When we talk about diversity, equity and inclusion in the workplace, many people immediately think about diversity in race, age, or gender. Today, I would like to talk about diversity in thought and information processing and how to make sure we are inclusive to everyone.
For the first 17 years of my life, I did not know that I had ADHD. I knew that I was not like all my classmates and teammates and that I processed information differently. However, I thought it was my fault and that I just needed to try harder. At the time, people were not aware of how ADHD can present in various ways, so it was assumed that I did not have it. After receiving my diagnosis, I panicked and thought my dreams might be unreachable because of it. Over the next few months, I learned more about how people receive and process information, as well as how these differences can lead to some amazing successes in life. There are amazing people who have had success and are navigating the world with ADHD, such as Simone Biles, Albert Einstein, Bill Gates, Michael Jordan, and more.
There are barriers to achieving this success and actions we take each day can make it easier for people to overcome those barriers. It is important to remember that when you are communicating with others, you may be giving them the same message, but it may need to be delivered differently. Clear and personalized communication benefits everyone, especially those who may be neurodiverse.
Some strategies to clarify your communication and help accommodate the neurodiverse population include:
1. Reflect on the appropriate method of communication. There are multiple methods of communication, and while a text message might be great for one person, a meeting might be better for another. People feel supported and heard if you ask what their preferred method of communication is.
2. Identify your purpose or call to action. With this communication, what are you trying to accomplish? Is it informative or is there a task that needs to be completed? Clearly identifying the call to action or purpose and highlighting that early in the communication can help people know what to keep in mind when reviewing the information.
3. Provide written deadlines and expectations. Even if you initially have a phone conversation with someone, following up with written deadlines, expectations, and instructions can help ensure that everyone is working towards the same goal and timeline.
4. Reduce stigma. Many people with ADHD struggle with whether they should disclose their diagnosis in the workplace out of fear it could lead to stigma and discrimination. You can work to promote a sense of inclusivity and openness within your workplace.
It is essential as working professionals, but also as those in healthcare and recruitment, that we increase our inclusivity and promote diversity in thought.
In the busy summer season for Physician Recruitment, it’s crucial to find a balance between productivity and well-being. Work-life balance is not just a trendy term; it’s essential for maintaining high performance and preventing burnout in this fast-paced industry. Here are some effective strategies for maintaining balance, boosting productivity, and promoting resilience during this important time:
First, make sure to discuss the expectations with leadership about the summer recruitment season. Keep senior management updated on market conditions and the need to promptly respond to candidate inquiries. Emphasize the importance of setting clear hiring goals to make decision-making processes more efficient and ensure timely engagement with candidates.
Review your recruitment workflows regularly to identify any bottlenecks and inefficiencies. It’s important to note that summer vacations can disrupt timelines, so it’s a good idea to implement strategies to maintain momentum during this time. Consider utilizing analytics from recruitment platforms such as PracticeLink and Doximity to optimize your job postings and outreach efforts. These tools can provide valuable insights into candidate preferences and market trends, giving you a competitive edge in recruitment.
Remember to fully embrace technology tools to increase productivity and streamline recruitment processes. Automated scheduling tools for emails and texts enable seamless communication, even when team members are unavailable. Platforms like PracticeMatch provide comprehensive data analytics to refine recruitment strategies and effectively target specific candidate demographics.
Maintain ongoing communication with past recruits to gather feedback on their experience and insights into workplace dynamics. Use these conversations to assess retention factors and identify areas for improvement. Building strong relationships fosters trust and loyalty, enhancing the organization’s reputation and attractiveness to prospective candidates.
Encourage team members to prioritize mental health by scheduling regular breaks and engaging in activities that promote relaxation and rejuvenation. Incorporate mindfulness practices into daily routines to alleviate stress and maintain focus. A refreshed mind contributes to sharper decision-making and sustained productivity throughout the recruitment process.
It’s crucial to acknowledge the significance of balance and resilience in retaining talent within the competitive physician recruitment industry. Organizations can reduce turnover rates and ensure long-term success by giving priority to employee well-being and operational efficiency. Investing in professional development and creating supportive work environments enhances employee engagement and organizational resilience.
As we dive into the summer recruitment season, it’s important to approach it with a good balance of productivity and well-being. To make the most of this season, recruitment professionals can focus on open communication with leadership, streamlining processes, making the most of technology, nurturing relationships, prioritizing mental well-being, and building long-term resilience. These strategies will help us achieve our goals while also taking care of ourselves.
Diversity, equity and inclusion (DE&I) play an important role in healthcare providers’ ability to deliver care that meets their communities’ needs. Building a diverse healthcare system starts with the provider recruitment professionals, their strategies and their processes. With DE&I embedded in workforce strategies, recruitment professionals can help foster more inclusive, representative hiring practices and ultimately, clinical staffs that are more reflective of the communities they serve.
While the ever-changing recruitment landscape requires continuously evolving tactics, these four practices act as a crucial foundation for sourcing, screening and hiring diverse candidates into the workplace.
Building a diverse healthcare system isn’t possible without developing diverse and inclusive sourcing and screening strategies. First, it’s important to evaluate your current recruitment strategies, such as where positions are posted and how positions are being promoted, to understand what’s working well and which methods can be improved. By implementing a diverse and inclusive mix of sourcing channels and an equitable screening process, you’ll be able to reach a wider variety of backgrounds and experiences, adding diversity to the candidates you’re interviewing as well as a broader set of skills and knowledge.
Active listening is a crucial aspect of the recruitment process. One of the first questions you should ask during the conversation should be about the candidate’s motivators, their interests and what is important to them – both professionally and personally. The answers to these questions will allow you to better understand your candidate and how they fit into your community and the organization. It will also help recognize potential barriers as well as any implicit and unconscious bias types. It’s important to hire individuals that recognize the significance of DE&I and ones that will prioritize these practices within their workplace.
Part of leadership’s role is to coach internal hiring authorities and recruitment professionals on inclusion and diversity policies within the healthcare industry. However, it’s also important for provider recruitment professionals to put in time outside of the workplace to stay up to date on DE&I industry standards and best practices through opportunities like conferences, memberships and certifications.
Professional certifications can give recruitment professionals added credibility within their organizations and the expertise to create more effective strategies. Certifications typically represent a higher level of expertise and require meeting specific standards, often set by professional associations (such as AAPPR). Typically, certifications require continuing education to maintain the certification and require those who hold the certification to periodically renew it.
In April 2022, AAPPR launched the Diversity, Equity and Inclusion Micro Certification Course, specifically to help recruitment professionals advance their DE&I strategies. This advanced certification for those already holding a current CPRP certification provides recruiters with tools they need to create a more diverse and inclusive environment within their respective organizations.
Recruitment professionals have the opportunity to help shape the future of healthcare and advance diversity and inclusion within our community. With a national physician shortage continuing to create challenges in recruitment, it’s crucial to invest in building a diverse healthcare system, and these four approaches are a great first step in doing so.
If you’re an AAPPR member, our organization offers various resources to support your recruitment strategies, and if you’re not an AAPPR member, you can become one today by visiting https://aappr.org/join-now/.
AAPPR’s annual conference, Advancing Connections, took place March 24-27 in Virginia Beach and brought together more than 1,000 recruitment professionals, sponsors and exhibitors to discuss important topics in physician and provider recruitment. The conference included educational keynote presentations, breakout sessions and roundtable discussions from healthcare leaders and featured discussions on various trending topics including diversity, equity and inclusion, artificial intelligence and the changing demands of physicians. Here are three key takeaways from this year’s conference:
DE&I needs to be embedded into recruitment strategies and every action your organization takes. The people hired into physician roles are crucial to the overall health of our communities. If a physician has an implicit bias toward patients, this implicit bias becomes the foundation of the organization and ultimately affects the care that is being delivered. We must build organizations where inequality is neither allowed nor tolerated, and that starts with the recruiters. Every patient – no matter their race or gender – needs to be taken seriously and provided with equal care.
The rise of AI is inevitable and should not be feared, but it is important to be aware of how it’s affecting the future of recruitment. There are ways to use AI to make recruitment strategies more efficient; however, the human elements of the profession, such as effective communication, empathy and intuition, cannot and should not be replaced. Although AI can be used to help streamline the hiring process through candidate matching, chatbots and automated scheduling, recruitment professionals need to be conscious of its potential negative impact on DE&I. AI is only as good as the data it receives, and it will require careful monitoring to make sure there is fairness in its outcomes. Because of this, we must be responsible in how we pursue and implement AI.
Despite the many generational differences in physician and provider priorities, there are a few common denominators: work-life balance, paid time off, location and compensation. Since the COVID-19 pandemic, the desires, wants and needs of physicians have shifted significantly. The five-day work week is no longer the norm – many are seeking hybrid work arrangements and ways to integrate their personal life with their work life. As the national physician shortage continues, it’s important to address these demands through the recruitment process. The recruiter’s role is to better understand each individual, their desires and what incentives they gravitate toward. Meeting these demands is where the competitive advantage lies and how you add to your culture and attract talent best suited to your organization.
Save the date for next year’s conference in Phoenix, Arizona! Pre-conference workshops will take place March 22-23, 2025, followed by the full conference on March 23-25, 2025.
In the heart of healthcare, where every recruitment decision can touch countless lives, lies an incredible opportunity—not just for professional growth, but for genuine connection and mutual support. It’s in this spirit that I want to talk about our journey at AAPPR and how we’re not just navigating this path, but thriving on it, together.
AAPPR’s latest strategic plan isn’t just a blueprint for the future; it’s a testament to our collective resolve to elevate our profession. It’s about recognizing the power of community and the undeniable impact we can have when we come together. Whether you’re stepping into the world of healthcare recruitment, or you’ve been guiding its evolution for years, there’s something deeply empowering about knowing your part of a community that genuinely cares about your growth and success.
So, how do we keep this community thriving, you ask? Well, it’s all about coming together, both in person and virtually, to connect with fellow AAPPR members. These events are our chance to swap stories, celebrate wins, and dive into the nitty-gritty of what’s working (and what’s not). It’s like a big brainstorming session, packed with fresh ideas, innovations, and a whole lot of inspiration to fuel your journey forward.
Our online community, AAPPR Chat, is like stepping into a lively coffee shop where conversations are brewing around every corner, ready to spark new ideas and insights. And if you’re looking for a more intimate setting, our regional Shared Interest Groups (SIGs) are like cozy nooks where you can dive deep into the intricacies of our field with like-minded peers.
Our virtual roundtables are where the heart of our community beats the loudest, bringing to the forefront the pressing issues we face and the collective wisdom we hold. And for anyone seeking a guiding light or looking to be one for others, our Mentor Match program embodies the essence of paying it forward.
This is more than just a strategic plan. It’s a reflection of our shared vision to not just advance in our careers but to do so with a sense of belonging, understanding, and shared purpose. So, let’s take this journey together, with open hearts and minds, ready to support each other every step of the way. Because at AAPPR, we’re not just colleagues; we’re a community, committed to not just navigating but thriving in the ever-evolving landscape of healthcare recruitment.
The process of recruiting physicians and advanced practice providers is highly nuanced. Recruitment professionals must leverage broad skills to attract, hire, and retain clinical talent. Did you know this process has a formal name? At the Association for Advancing Physician and Provider Recruitment, we refer to it as the Recruitment Continuum.
By definition, a continuum is a coherent whole characterized as a collection, sequence, or progression of values or elements varying by minute degrees. In other words, it represents a gradual progression from one point to another without distinct, sharp boundaries. Continuums are commonly used in various science, mathematics, and philosophy fields to understand and describe phenomena that vary across a spectrum rather than being discrete or categorical. In the field of physician and provider recruitment it represents the nuanced recruitment process that flows seamlessly from one phase to another.
For recruitment professionals, understanding and using the continuum concept helps them in a process where there is a gradual transition from one phase to another. This means there are no clear breaks or gaps between the different points on the continuum; the process should be smooth and incremental.
The provider recruitment continuum begins with sourcing and ends with retention.
Source: identifying and/or building a provider prospect pool and creating awareness of/interest in practice opportunities.
Screen: the internal process of pre-qualifying candidates to meet organizational/provider expectations, which may include interviews and site visits.
Select, Offer, and Hire: identifying and selecting the best-fit candidate through the extension and closing of an offer.
Onboard: the continuance of the recruitment process to meet onboarding timelines and standards, ensuring successful entry and integration into practice and community.
Retain: data analysis, strategic alignment, and program implementation with the intent of promoting provider satisfaction, resulting in increased retention.
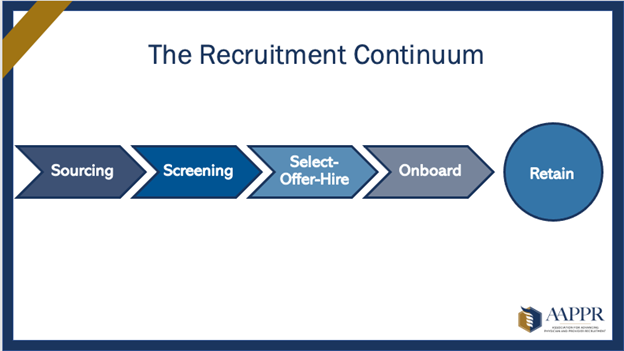
Through a continuum, candidates experience a seamless transition from one phase to another throughout the recruitment process, with no apparent breaks or gaps between the different stages. While recruitment professionals must leverage diverse skills to attract, hire, and retain clinical talent effectively, candidates must have an easy and smooth experience. By looking at the steps in the recruitment process as a continual progression, we can ensure that recruitment professionals can practice to the best of their ability and that candidates have a positive experience.
AAPPR uses cookies for functional and analytical purposes. By continuing to browse or by clicking “Accept,” you agree to the storing of cookies on your device to enhance your site experience. To learn more about how we use cookies or how to change your settings, please see our privacy policy.
Accept Close